Lung cancer cases among non-smokers are increasing at an alarming rate, according to a new study published in The Lancet Respiratory Medicine journal. The research, released on World Cancer Day, February 4, highlights that air pollution may be a major factor behind this growing trend. The study found that adenocarcinoma, a form of lung cancer originating in glandular cells, accounted for 53-70 percent of lung cancer cases among non-smokers worldwide in 2022. Unlike other lung cancer types, adenocarcinoma is weakly linked to cigarette smoking, making environmental and genetic factors more significant contributors to its development.
The study emphasizes that while smoking remains the primary risk factor for lung cancer, an increasing number of cases are emerging in individuals who have never smoked. Researchers suggest that prolonged exposure to air pollutants, including fine particulate matter (PM2.5), can trigger genetic mutations that lead to cancer. Urban populations, especially those living in industrial regions with high pollution levels, appear to be at greater risk. Experts warn that indoor pollutants, such as secondhand smoke, cooking fumes, and radon gas, could also be driving the rise in lung cancer among non-smokers.
Genetic predisposition may play a role in the susceptibility of certain individuals to lung cancer. Some people may carry inherited mutations that increase their risk of developing adenocarcinoma despite the absence of traditional risk factors. The study notes that women are more likely than men to develop lung cancer without a history of smoking, suggesting potential hormonal or genetic influences. Scientists are now investigating how these biological factors interact with environmental exposures to cause lung cancer.
Lifestyle factors and occupational hazards further complicate the picture. Exposure to carcinogenic chemicals, including asbestos, diesel exhaust, and industrial solvents, has been linked to increased lung cancer risk. People working in construction, mining, and manufacturing industries face higher exposure to these harmful substances, which can contribute to lung damage over time. The study suggests that strict workplace regulations and improved air quality standards are necessary to reduce the impact of these risk factors.
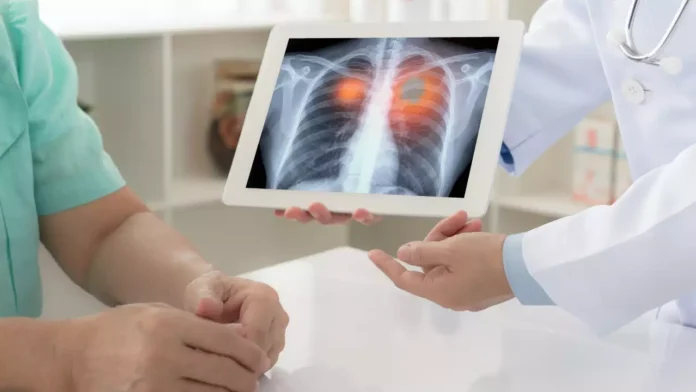
Early detection remains crucial in managing lung cancer cases effectively. Since symptoms such as persistent cough, shortness of breath, and chest pain often appear at later stages, regular screenings can help identify cancer before it spreads. Low-dose computed tomography (LDCT) scans are increasingly being recommended for high-risk individuals, including those exposed to air pollution or with a family history of lung cancer. The study urges governments and healthcare organizations to implement widespread screening programs to improve early diagnosis and survival rates.
Medical advancements are providing new hope for non-smokers diagnosed with lung cancer. Targeted therapies and immunotherapy have shown promise in treating adenocarcinoma by attacking specific genetic mutations that drive cancer growth. Personalized treatment plans based on genetic testing are improving patient outcomes, with many individuals responding well to these innovative approaches. Researchers are also exploring new drug combinations that could enhance the effectiveness of existing treatments.
Raising awareness about non-smoking-related lung cancer is essential to changing public perception and promoting proactive health measures. Many people still associate lung cancer primarily with smoking, leading to delayed diagnoses in non-smokers. Educating individuals about alternative risk factors and encouraging routine health checkups can help bridge this gap. Experts recommend that people living in high-pollution areas take precautions such as using air purifiers, wearing masks in heavily polluted environments, and reducing exposure to indoor pollutants.
Healthcare professionals stress the importance of a holistic approach to lung cancer prevention. Governments must strengthen policies to reduce air pollution and enforce stricter environmental regulations. Investing in clean energy solutions, promoting sustainable urban planning, and reducing industrial emissions can significantly lower the risk of lung cancer in future generations. The study calls for global cooperation in tackling environmental threats that contribute to lung disease, urging policymakers to take decisive action.
With lung cancer cases rising among non-smokers, proactive measures are necessary to address the underlying causes. Understanding the link between air pollution, genetic susceptibility, and lifestyle factors can pave the way for effective prevention and treatment strategies. Regular screenings, improved healthcare policies, and continued medical research will play a critical role in combating this silent but growing health crisis.
Researchers are also exploring the potential role of diet and nutrition in lung cancer development among non-smokers. Some studies suggest that chronic inflammation caused by poor dietary choices may contribute to cellular changes that increase cancer risk. Diets rich in antioxidants, found in fruits, vegetables, and whole grains, may help reduce oxidative stress and protect lung tissue from damage. However, more research is needed to determine the exact relationship between nutrition and lung cancer in non-smokers.
Mental health considerations are becoming an important aspect of cancer care, particularly for non-smokers who receive a lung cancer diagnosis. Many patients struggle with confusion and stigma, as the disease is often associated with smoking. Psychological distress can impact treatment outcomes, making it essential for healthcare providers to offer emotional support alongside medical care. Counseling services and patient support groups can help individuals navigate the emotional challenges that come with a lung cancer diagnosis.
Emerging studies are also investigating the role of the microbiome—the collection of bacteria and microorganisms in the body—in lung cancer development. Some researchers believe that an imbalance in lung microbiota could create an environment that promotes cancer growth. While this field is still in its early stages, future breakthroughs could lead to innovative treatments that target microbial imbalances to slow or prevent lung cancer progression.
Technological advancements in diagnostics are offering new hope for early lung cancer detection. Liquid biopsies, which analyze cancer-related biomarkers in blood samples, are gaining traction as a less invasive alternative to traditional tissue biopsies. These tests have the potential to identify lung cancer at an earlier stage, improving survival rates and allowing doctors to tailor treatments more effectively. As research in this area progresses, liquid biopsies may become a routine part of lung cancer screening programs.
Addressing lung cancer in non-smokers requires a collective effort from governments, healthcare professionals, and the public. Greater investment in clean energy, improved air quality standards, and advancements in cancer research will be crucial in tackling this growing health challenge. As awareness increases, early detection rates may improve, leading to better treatment outcomes and a deeper understanding of the disease.