The blood scandal that rocked the UK is one of the gravest public health disasters in the nation’s history, leading to the infection of approximately 30,000 people and causing around 3,000 deaths. This tragedy unfolded during the 1970s and 1980s, leaving a lasting impact on countless lives and prompting significant changes in medical protocols and public health policies.
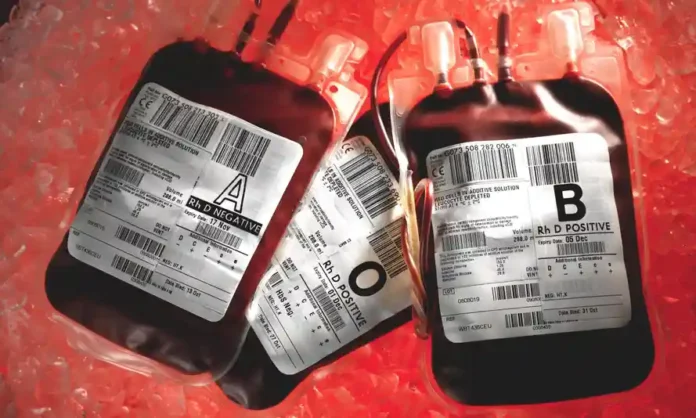
The root of the scandal lies in the treatment of hemophilia, a genetic disorder that impairs the blood’s ability to clot. To manage this condition, patients were treated with clotting agents derived from human plasma, known as Factor VIII and Factor IX concentrates. These concentrates were made from pooled blood plasma, often sourced from multiple donors. At the time, the UK was unable to meet the demand for these products domestically and thus imported supplies from the United States.
The US-sourced plasma was problematic. During the 1970s and early 1980s, the United States collected blood from high-risk populations, including prison inmates and intravenous drug users, who were more likely to carry blood-borne viruses such as HIV and hepatitis C. Due to inadequate screening and testing procedures, many batches of plasma were contaminated. Patients in the UK receiving these contaminated blood products were unwittingly exposed to these viruses. It is estimated that around 30,000 people were infected with hepatitis C, and approximately 1,500 hemophiliacs were infected with HIV. The hepatitis C infections alone resulted in significant morbidity and contributed to the deaths of around 3,000 individuals.
The response to the unfolding crisis was slow and marred by systemic failures. Many victims were unaware of their infections for years due to the slow development of symptoms associated with hepatitis C. Moreover, the government’s reluctance to fully acknowledge the extent of the contamination and provide timely compensation added to the victims’ plight. The scandal was exacerbated by alleged attempts to cover up the severity of the situation. Reports indicate that documents detailing the risks of using imported blood products and the extent of contamination were destroyed or withheld. The perceived lack of transparency and accountability fostered deep mistrust between the affected communities and the authorities.
The blood scandal led to numerous legal battles and inquiries. Victims and their families sought justice and compensation through the courts, facing prolonged and arduous legal processes. In 2017, after decades of campaigning by victims and advocacy groups, the UK government announced a public inquiry into the scandal, led by Sir Brian Langstaff. The inquiry, which began in 2018, aimed to investigate the circumstances surrounding the use of contaminated blood products and the handling of the crisis by the government and health authorities. It examined evidence from thousands of witnesses, including victims, medical professionals, and government officials. The ongoing inquiry has been crucial in uncovering the truth and providing a platform for those affected to share their experiences.
The blood scandal has had a profound and lasting impact on public health policy and practices in the UK. It underscored the importance of stringent screening and testing of blood products, leading to significant reforms in blood donation and transfusion protocols. The tragedy also highlighted the need for greater transparency and accountability within public health systems. Moreover, the scandal has raised awareness about the risks associated with blood products and the importance of supporting victims of medical disasters. It has prompted calls for improved compensation schemes and better support mechanisms for those affected by similar crises.
The UK’s blood scandal remains a stark reminder of the devastating consequences of inadequate safety measures and the failures of governmental oversight. While the ongoing public inquiry seeks to bring justice and closure to the victims, the lessons learned continue to shape public health policies to prevent such a tragedy from recurring. The scandal not only underscores the critical need for rigorous medical standards but also the moral imperative of transparency and accountability in protecting public health.